Queen Elizabeth tests positive for covid19 - what early treatments will she be getting - will those be advertised to the public? (Feb 20, 2022)
Will it include Ivermectin, or at the very least steroids-at-day8 to avoid risk of death, and avoid risk of long haulers?
UPDATE: It seems she has some post-covid19 residual fatigue still - see:
https://stereomatch.substack.com/p/update-to-queen-elizabeth-post-evidently
.
DISCLAIMER: these are recommendations for doctors - and should not be taken as gospel - viewers need to follow FLCCC recommendations and that of other early treatment doctors - that they have the drugs needed for covid19 in their medicine cabinets ahead of time - i.e. secure a telehealth consult and have the drugs available at home.
Reason: once you are sick it becomes logistically difficult to secure the drugs needed in time - as time for procuring from pharmacist, time to get consult with a doctor can vary.
The advantage of having drugs available is that Ivermectin can be taken immediately on appearance of an index case in a household or place of work (post-exposure prophylaxis), and Prednisolone is a life saver when taken not earlier than day7-8 (don't want to suppress immune response while live virus is still in large numbers) and not much later than day7-8 (live virus is near zero by day7-8 - see MATH+ extended PDF) when hyperinflammatory stage starts up like clockwork.
Lack of access to steroids-at-day8 is a major risk factor for severe disease and long haulers. In fact, in large protocol-driven hospitals the use of 6mg Dexamethasone (capped) + Remdesivir is problematic not just because of the Remdesivir at late stage (and Remdesivir-associated risk of kidney failure), but because of the "capped" steroids protocols that many large hospitals use.
This is borne of an erroneous reading of the RECOVERY UK trial for steroids which just happened to use 6mg Dexamethasone. This trial also gave a small signal that steroids may be harmful if given before intubation - this probably stems from bad grouping of very early patients given steroids in the group. Because delaying steroids until intubation is putting the cart before the horse. In contrast, if steroids are given at day8 in sufficient quantity, it quells the hyperinflammation and things don't proceed to hypercoagulability.
This capping to 6mg Dexamethasone is a killer - since this is barely enough to reverse a day8 person. 6mg dexamethasone is equivalent to 40mg prednisolone - which is what is given to a day7-8 person - and sometimes even this needs to be escalated to 60mg or 80mg prednisolone in some rapidly declining cases.
If a day10 person at oximeter 90 or lower arrives in hospital, 40mg prednisolone (6mg dexamethasone) will not turn them around fast enough. They will stagnate, be "observed" for a few days and then wind up on ventilator.
This is probably the reason why death rate at large US hospitals is 22-25pct and for their ICUs 80pct - compare this to FLCCC protocol-driven hospitals like Dr Joe Varon's and Dr Paul Marik's (prior to interference by Sentara Hospitals) where both these metrics are halved.
Early treatment doctors who get to patient before day8 manage to achieve near zero deaths and zero long haulers on a routine basis - doctors who have treated 3000-4000 covid19 patients with near zero deaths.
EDIT: Mar 1, 2022 - if hospital staff is constrained by hospital protocol to not escalate steroids beyond 6mg Dexamethasone, they should consider starting Fluvoxamine early - and failing that starting Cyproheptadine at day8 onwards - for reduced need for high dose steroids - see the section on Cyproheptadine below.
.
End of Disclaimer
.
.
Summary: Queen Elizabeth has tested positive for covid19.
Presumably she has been started on early treatment even before her covid19 PCR test or rapid test was found to be positive.
The New York Times article is at the bottom.
.
Short primer on viral timeline
Delta:
1 - exposure
2
3
4 or 5 - day1 of symptoms (live viral load is at max)
day2 of symptoms
day3
day4
day5 live viral load is near zero for many patients
day6
day7 - live viral load is near zero for nearly all patients - consider starting on precautionary steroids-at-day7-8 protocol
.
Omicron:
1 - exposure
2
3 - day1 of symptoms (live viral load is at max) -
day2 of symptoms
day3
day4
day5 live viral load is near zero for many patients
day6
day7 - live viral load is near zero for nearly all patients - consider starting on precautionary steroids-at-day7-8 protocol
.
.
Caveat on "live virus is near zero by day8"
(Added Feb 22, 2022)
The live virus falls to low levels by day5 in some, and by day8 in most - as explained by FLCCC and Dr Paul Marik in interviews.
Part of this could be due to lack of availability of new ACE2 rich cells to target. As all the accessible ones are exhausted. This may lead to slowdown of expansion of live viral load - allowing the ramping up of the adaptive immune arm to catch up.
The viral debris triggers an inflammatory response - and by day7-8 this hyperinflammatory response starts to become visible (see above for post-day8 hyperinflammatory signals).
If this post-day7-8 hyperinflammation is not quelled, it leads to inflammation in micro-capillaries and leaky blood vessels - and potential expansion of the little remaining live virus to new areas of the body. Thus providing the virus with new ACE2 rich cells to infect.
The inability to arrest the post-day8 hyperinflammatory stage may be directly responsible for a reemergence of live virus post-day8.
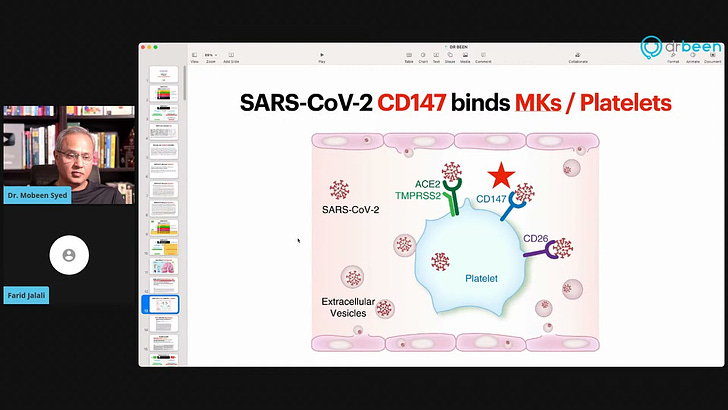
In addition, an inability to arrest the post-day8 hyperinflammatory stage allows for inflammation to run rampant which can lead to release of clotting factors by lining of blood vessels. In addition, the platelets (which are stores of serotonin) can release large amounts of serotonin which can lead to clotting.
Once the live virus is given opportunity to expand to new areas of the body, it can continue to persist in immuno-protected areas of the body - like the brain - or in areas where there is rapidly turnover of cells - like the gut - where the virus can contiue to find new ACE2 rich cells as targets.
If a patient is treated with Ivermectin by day1-7 onwards and with steroids-at-day8 (at sufficient dose to quell the post-day8 hyperinflammatory stage), then the live virus remains less of a concern and will be eliminated.
The proof of this is that patients who receive steroids-at-day8 have zero long haulers syndrome.
Some may have residual anosmia or fatigue - but these can be addressed using refresher courses of Ivermectin as described elsewhere here.
So if early treatment and followup is done responsively to the condition of the patient, there should be zero deaths, and zero long haulers.
.
.
Omicron mild day1-7 with early treatment, but be wary of long hauler risk
For Omicron, if one of the early treatment alternatives for day1-7 are given, then for Omicron, symptoms will be less, and may have 101 F fever on day1 and then going down to normal by day3-4.
Despite a "mild" day1-7, there remains a risk of long covid19 with Omicron (from current information - I am hearing from early treatment doctors about such a risk).
The risk may be less compared to Delta - but so far indications are that there is some hyperinflammatory signal at day7-8 with Omicron in some patients - which is a sign that there may be some type of long hauler symptoms with Omicron.
Given that Omicron will infect everyone - this could create a large pool of long haulers out of the Omicron infection.
And this applies to those previously unvaccinated, 2 dose vaccinated, and even 3 dose boosted.
I have seen a 3rd dose Pfizer boosted individual have pulse rate 123 at day7 (even though he had post-exposure prophylaxis and thus showed no symptoms day1-7 - like others in the household who were 2 dose vaccinated but not boosted).
There was a subtle oximeter dip in some cases. With accompanying reduction in stamina for walk etc.
Less severe than Delta - but which has potential to mature into long covid19 in 2 weeks (due to creeping inflammation - see below).
.
.
Multiple alternatives for day1 onwards
During day1-7, I am assuming she is being treated with one of these:
.
- Ivermectin + Famotidine + Zinc + Vitamin D3 + C + B1 + Aspirin + NAC
.
Ivermectin - 0.4mg/kg bodyweight for 5 days or longer (plus in the post-day8 period, a refresher course may be given for residual anosmia/fatigue - see below) (some early treatment doctors who don't give steroids-at-day8 may as a precaution continue Ivermectin beyond the 5 days up to 10 days - though in such cases if there are side-effects i.e. dizziness (low blood pressure) then should be reduced or stopped)
Famotidine (Pepsid - H1 blocker antihistamine) - 20mg+20mg for 5-10 days
Zinc - 50mg elemental zinc (about 220mg zinc sulphate or 360mg zinc gluconate) - see: https://saidit.net/s/Ivermectin2/wiki/index#wiki_zinc_-_elemental_zinc). Here is the elemental zinc in different zinc compounds: zinc sulfate 220mg has 50mg elemental zinc - zinc gluconate 50mg has 7mg elemental zinc.
Vitamin D3 - 200,000 IU - one time - then 5000 IU per day
Vitamin C - 500 to 1000mg per day
Vitamin B1 (Thiamine) - 100mg - as immunomodulator
Vitamin B-complex
Aspirin 75mg (for day1-7 - if catch patient late, then may need more)
NAC - 400mg+400mg per day
For additional supplementation like Melatonin etc. - see: FLCCC I-MASK+ protocol: https://covid19criticalcare.com/covid-19-protocols/i-mask-plus-protocol/
Also see the FLCCC MATH+ extended PDF: https://covid19criticalcare.com/wp-content/uploads/2020/12/FLCCC-Protocols-%E2%80%93-A-Guide-to-the-Management-of-COVID-19.pdf
.
- H1/H2 blocker antihistamines (Dr Shankara Chetty protocol)
.
- Fluvoxamine or (Fluvoxamine + Ivermectin) (Dr Syed Haider, Text2MD protocol - and part of FLCCC I-MASK+, MATH+, I-RECOVER protocols)
.
Typically Fluvoxamine 50mg+50mg per day
or if side effects, switch to Fluoxetine (Prozac) 30mg daily
Above dosage from FLCCC MATH+ protocol: https://covid19criticalcare.com/covid-19-protocols/math-plus-protocol/
However, some doctors may prescribe higher or lower doses - depending on patient tolerance for Fluvoxamine (since some people do not like it and will discontinue using it - in that case switch to Fluoxetine as FLCCC/Dr Syed Haider suggests, or switch back to full FLCCC protocols)
.
.
If Ivermectin is not available
If Ivermectin is not available, or your doctors are not comfortable giving it, then one of the other treatment alternatives above will also suffice.
As long as you have access to steroids-at-day7-8, one can mitigate the worst outcomes with timely intervention against the post-day8 hyperinflammatory stage.
FLCCC I-MASK+ protocol suggests as alternative or as addition - for 14 days:
Nigella Sativa (black cumin seed) - 40-80mg/kg bodyweight
Honey - 1gram/kg bodyweight daily
See: https://covid19criticalcare.com/covid-19-protocols/i-mask-plus-protocol/
Nigella Sativa + Honey have shown good results in some studies. See: https://c19ns.com/
.
.
Avoiding risk of hyperinflammation post-day7-8 - steroids-at-day7-8
At day7-8, I presume her doctors will be watching for signs of hyperinflammatory stage:
oximeter daily decline
pulse rate in 90s or 100+ at rest (even without fever)
anomalous return of fever on day7-8 ("hyperinflammatory fever")
And start her on steroids (40mg Prednisolone or higher) - escalating as needed to show daily oximeter improvement.
Once oximeter shows improvement 1-2 points next day - that usually is a sign that steroids dose is sufficient and patient will be at oximeter 99 in 3-4 days and feeling fully fit.
Typical duration of steroids-at-day7-8 protocol would be 40mg Prednisolone for 1 week - then taper to zero over next week.
Usually this is sufficiently long to bypass the inflammatory period.
I have observed cases where patient started steroids-at-day7-8 and then in 3 days was feeling great with oximeter at 99 - and wanting to go to gym (dissuaded from doing so). And they stopped steroids (since feeling great). The hyperinflammatory fever returned - they got scared and started steroids again - fever went away.
So physicians giving steroids for just 3 days (as has been reported by some patients) are being extremely conservative - and risking long haulers syndrome for their patients.
.
.
Duration of Ivermectin - 5 days or more?
(Added Feb 22, 2022)
While I mention Ivermectin 0.4mg/kg bodyweight per day for 5 days - it can be extended for more days - especially if patient is not feeling any side effects from Ivermectin i.e. no dizziness/low-blood-pressure (or visual disturbances).
About 1 in 20 patients do experience some dizziness - usually can reduce dose to 0.2mg/kg and these issues go away.
Sometimes prolonged period of Ivermectin use (or high dose) can also lead to visual disturbances (starry eyed type of feeling). This also goes away when reduce dose or stop Ivermectin within day or two.
But there can be a subset of patients who don't want to take even 0.2mg/kg. For these will just have to manage with the other drugs and then steroids-at-day8.
Sometimes one can give Ivermectin 0.4mg/kg bodyweight for 5 days - and then take a break - esp. if you know you will be doing a refresher Ivermectin course later i.e. after started steroids-at-day8 - this Ivermectin course is often needed if patient has residual anosmia (taste/smell loss) or fatigue.
In addition after the steroids are over, the patient will be doing the post-covid19 protocol mentioned here - where they would be taking Ivermectin 0.4mg/kg bodyweight every Sunday i.e. weekly.
These decisions to continue Ivermectin in some form for longer are made in order to secure a wider safety margin - to protect from possible rare cases of viral persistence, or continuing spike protein presence.
Ivermectin is thought to neutralize the impact of spike proteins - and if it's use is not bothering the patient, an early treatment doctor can choose to err on the side of caution and give Ivermectin for longer, according to situation.
Feedback on this document from early treatment doctors
Some early treatment doctors have provided feedback that they continue Ivermectin well beyond 5 days (see Acknowledgements section and Twitter thread at bottom).
And give for 10-14 days (although after first 5 days they may taper down to lower dose per day - esp. if patient seems to be improving at these doses).
The rationale for this is to keep a safety margin and protect against the possibility that live virus is persisting in some rare case.
However many early treatment doctors don't give steroids-at-day8 as a matter of course - usually only to those who are feeling some oximeter decline at day8 etc. This stems from a general wariness of using steroids.
In the protocol described here, steroids-at-day7-8 is always given (even for "mild" cases - since even for mild if skip steroids-at-day8, a subset will get "creeping inflammation" which matures into full blown day8-like hyperinflammation in 2 weeks - this may be the path for how asymptomatic/mild cases can become long haulers).
Once steroids-at-day7-8 are started, a lot of the pressure on the doctor subsides - as the fear of being late in starting steroids goes away. Patient will be exposed to steroids for 1 week and 1 week of tapering to zero. Usually this is a short enough course to not have major issues.
Most symptoms should be reduced by day8, and any remaining should go away once start steroids-at-day7-8.
The day1-7 symptoms usually have gone by day7-8 - if some remain like vomiting, or stomach issues or incessant cough - those go down once steroids-at-day7-8 are started.
For this reason sometimes just a 5 days course of IVM may be enough - esp. since post-day8 you will be giving a refresher course of IVM 0.4mg/kg bodyweight per day for 3 days - to address any residual anosmia/fatigue. And if there is partial reversal of anosmia/fatigue - then an extra refresher course may be given after one week gap.
In addition, in post-covid19 period (after steroids tapered to zero) - the patient will be given a post-covid19 protocol of Ivermectin, Aspirin and NAC (see section below).
So if one is planning for a longer term use of Ivermectin, then one may stick to the 5 day course during day1-7, since more will be given after that.
However, if early treatment doctor wants to reduce chances of residual live virus etc. then could continue Ivermectin at a lower dose after the 5 day course has finished.
.
.
Post-covid19 protocol - 1 month caution
Post-covid19, her doctors should also consider for 1 month:
Avoid heavy exercise
Aspirin 75mg per day
NAC 200mg+200mg per day (antioxidant, glutathione replenishing and protective for lung)
Ivermectin 0.4mg/kg bodyweight - every Sunday (i.e. weekly)
Heavy exercise is associated with higher risk of long haulers.
Several doctors treating long haulers and long haulers themselves report how exercise exacerbates their symptoms.
Dr Bruce Patterson/Dr Yo (https://www.covidlonghaulers.com) have also commented on how exercise - and increased heart rate - seems to be associated with greater activation of symptoms for long haulers.
However, heavy exercise here seems to be relevant also because post-covid19 some subset of patients (who have not taken the steroids-at-day7-8 protocol) experience elevated heart rate (possibly pericarditis) - and these people need to avoid heavy exercise.
The Aspirin is suggested as a risk reducer for micro-clots. Usually micro-clots is a later stage when hyperinflammation has been allowed to run rampant. If steroids-at-day8 is done there seems to be reduced progression to hypercoagulability. However if hyperinflammation is allowed to run rampant, it will lead to endothelial dysfunction in blood vessels and release of clotting factors - or via serotonin syndrome like conditions (platelets releasing excess serotonin - leading to coagulation cascades). See Dr Been interview of Dr Farid Jalali for the role of Fluvoxamine early, and Cyproheptadine at day8 onwards to reduce risk of serotonin syndrome like conditions:
The NAC (N-acetyl cysteine) is suggested as a counter for any glutathione depletion (NAC is a precursor for glutathione - the body's master antioxidant). Depletion of glutathione may happen due to inflammation. Also NAC is generally suggested for recovery from lung damage in respiratory diseases. See Dr Roger Seheult (MedCram) videos on NAC and Glutathione:
https://www.youtube.com/watch?v=Dr_6w-WPr0w
- and:
https://www.youtube.com/watch?v=OtL0B1bqXak
.
.
Post-covid19 residual anosmia or fatigue reversal
Post-covid19 if there is some residual anosmia or fatigue - her doctors can consider this regimen:
Ivermectin 0.4mg/kg bodyweight per day - for 3 days
For anosmia will reverse within 1-2 days.
Also beneficial for residual fatigue.
If partial, do a refresher course after a week.
Anosmia reversal is one of the macro effects of Ivermectin use - i.e. it is one of the first and most obvious effects observed by early treatment doctors.
.
.
Post-day8 observation and aggressive treatment
Post-covid19 she should be monitored for signs of fatigue or hyperinflammation - and should be aggressively treated for that.
That is don't leave it to "observe" and stagnate - instead act early.
.
.
Avoiding risk of long haulers
I am assuming also that even if she does not show signs of hyperinflammation, she would still be started on a precautionary steroids course (or at least monitored closely for signs of ramping of inflammation).
Because those who don't get steroids-at-day8 - a subset of them show a creeping inflammation that in 2 weeks looks like full blown day8 type hyperinflammation.
In others who did not take steroids-at-day8 (because they skipped it) there can be a subset who show elevated heart rate which may persist (until the next time they take a steroids-at-day8 course).
I have seen both types of behaviors in those who did not take steroids-at-day8.
In patients who took steroids-at-day8 and saw improvement and in 3 days were thinking about going to the gym, and feel good enough that they stop steroids on their own - there can be a resurgence of hyperinflammatory signals - fever can return, the patient panics and restarts steroids, and the fever (hyperinflammatory fever) goes away.
So this too is a risk - some doctors who do start on steroids-at-day8 may give too short a course (not being familiar with viral timeline) - which may make the patient stagnate or get worse.
If her doctors have personal experience of alternatives to steroids which work just as well - for example Dr Darrell DeMello uses colchicine - then they can consider that as alternative.
.
.
In case of post-day8 oximeter at 93 or lower
If catch the patient late i.e. at day10 or oximeter is below 95 and declining daily, then add:
Cyproheptadine - 8mg - 3 times a day - Cyproheptadine usually should be started not much earlier than day7-8 and may not be needed for patients who are showing oximeter reversal with steroids alone. However for patients who have not responded to Prednisolone 40mg per day - Cyproheptadine may need to be added, and Prednisolone escalated as well - until oximeter reversal/improvement is clearly seen. With Cyproheptadine, patient will sleep and only wake up for meals (inconvenient for a mild patient, but not too bad for a patient who is at oximeter 93 or lower who is already exhausted) - do not stop Cyproheptadine suddenly but taper off. See Dr Been interview of Dr Farid Jalali for the role of Fluvoxamine early, and Cyproheptadine at day8 onwards to reduce risk of serotonin syndrome like conditions (see video above). Cyproheptadine is in the FLCCC MATH+ protocol: https://covid19criticalcare.com/covid-19-protocols/math-plus-protocol/
Inhaled Budesonide (steroids) - 4-5 times a day - will bring relief for incessant cough, and temporary relief for patient. Steroids dose is less than 1mg - so does not impact the systemic oral/intravenous steroids you are giving. Inhaled steroids provides targeted steroids dose for lungs and is very helpful addition. Usually inhaled steroids can be started when you start oral/intravenous steroids-at-day8 - however inhaled steroids can be started 2 days before that - i.e. should be safe to start day5. There is a group of doctors who have treated 7000 patients with near zero deaths - and they use inhaled steroids from the first day they see patient (so while I do not suggest this - it establishes a safety profile for earlier-than-day8 use of inhaled steroids - however I would suggest avoid giving earlier than day5 from first symptoms - unless patient is showing clear signs of incessant cough and possibility that is not at day5 but may have counted days wrong).
Prednisolone (oral steroids) - for a patient at oximeter 93 or at day 10 or more - usually Prednisolone 40mg will not be sufficient - and you may need to start at a higher dose (don't want to wait a day and then find out it was not enough - have lost another day) - so can start at 60mg or 80mg - and then taper as see oximeter reversal/improvement. If patient is not showing oximeter reversal/improvement daily, escalate steroids dose until it starts showing improvement - there is no advantage to "waiting" or "observing" - at the right dose of steroids, the patient shows immediate response by next day oximeter should be 1-2 points higher. Once that happens, it means the steroids dose is sufficient, and generally that 1-2 point oximeter improvement continues monotonically - and in 3-4 days the patient can be at oximeter 99. In cases at day10 or later, or with oximeter at 90 or lower - the recovery may take longer. And steroids may have to be continued more than the typical (1 week + 1 week to taper to zero) - and could take as long as 3 weeks. If patient is reversing but not as fast i.e. is stagnating at moderate oximeter levels but not fully recovering to 98-99 oximeter - may need to give high dose steroids (pulse dosing) every few days - for example if are giving 80mg - then could give 120mg every third day (split up doses for morning-lunch-dinner). Dr Pierre Kory recommends high dose pulse dosing of steroids to counter "organizing pneumonia" in covid19 - see the FLCCC MATH+ protocol - which uses up to 1000mg Prednisolone for 3 days as a "pulse dosing" to counter recalcitrant lung damage: https://covid19criticalcare.com/covid-19-protocols/math-plus-protocol/
other supplements in the FLCCC MATH+ protocol can be considered that are anti-inflammatory - Melatonin (anti-oxidant impact), statins (reduce micro-capillary inflammation).
Aspirin can be escalated, or anti-coagulants started (FLCCC recommends 325mg Aspirin or low molecular weight Heparin) while considering risk of bleeding.
.
.
EDIT: Mar 1, 2022
Low dose steroids hospital protocols may benefit from Cyproheptadine addition
As explained above, in hospitals which cap Dexamethasone (steroids) to 6mg - this works to save patients with low levels of inflammation (in the post-day8 hyperinflammatory stage) - however it is insufficient to save a patient with more severe inflammation.
If increasing steroids is not an option for a hospital or medical staff, then the alternative is to either start Fluvoxamine early (day1 of first symptoms onwards) - this seems to reduce the need for high dose steroids at day8 onwards.
Or failing that, if they are closer to day8 or later - then Cyproheptadine 8mg - 3 times a day.
If Cyproheptadine is given by day8 - then the need for steroids is reduced - i.e. 6mg Dexamethasone MAY work (when otherwise it may not have).
So in situations where hospital staff are prevented from escalating steroids, this may be an alternative strategy.
.
For Cyproheptadine here is a quote from Dr Syed Haider in a Dr Been video:
https://youtu.be/Md-y01JdxvE&t=3120
or
https://odysee.com/@DrMobeenSyed:1/dr.-syed-haider-discusses-covid-2:8?t=3120
at the 52:00 minute mark:
Pneumonia - used to give them lovenox (enoxaparin/low molecular weight heparin)
Nowadays I go to Cyproheptadine and that seems to reverse it pretty quickly
.
Both Fluxoxamine and Cyproheptadine are listed on the FLCCC I-MASK+/MATH+ protocols.
Dr Farid Jalali has documented many cases of reversal of lung issues with the use of Cyproheptadine (reversing serotonin syndrome-like conditions).
Dr AK Chaurasia from Uttar Pradesh also reports similar benefit from Cyproheptadine at day8 onwards. Dr Darrell DeMello from Mumbai, India has similar view: https://twitter.com/DarrellMello/status/1497873855850762243?t=Ly886VFHK1hXrRHIZQ4k8g&s=19
.
.
EDIT: Mar 1, 2022
Finding a doctor who understands early treatment
The r/ivermectin sub-reddit's wiki has a section on Early Treatment Doctors:
https://saidit.net/s/Ivermectin2/wiki/index#wiki_early_treatment_doctors
Some of the doctors mentioned have treated 3000-4000 patients with near zero deaths and near zero long haulers.
Early treatment doctors are often independent or have their own clinics - this is what distinguishes them from doctors in large US hospitals which have established rigid protocols like 6mg dexamethasone (capped) + Remdesivir. Often in order to continue to practice on a rigid protocol dictated by hospital administrators, the doctors wind up either leaving if they find it is killing patients, or staying and then justifying (perhaps more to themselves) why there is no other alternative available (after all they couldn't be killing people for 2 years without noticing if there was a better solution - right?).
Often the doctors who understand viral timeline, and have treated covid19 patients in large numbers are also the ones who understand long haulers (long covid19) and post-vaccine issues - many times the same drugs used in post-day8 hyperinflammatory stage are also beneficial for long haulers - Ivermectin, Famotidine, steroids, anti-coagulants etc.
.
.
Article:
.
https://www.nytimes.com/live/2022/02/20/world/queen-elizabeth-covid
or
non-paywalled mirror:
Live Updates: Queen Elizabeth Tests Positive for the Coronavirus
Feb. 20, 2022
The 95-year-old British monarch was “experiencing mild coldlike symptoms,” Buckingham Palace said. She recently met with her son Prince Charles, who had tested positive this month.
Here’s what you need to know:
Queen Elizabeth is infected with the coronavirus.
Britain was poised to end its pandemic restrictions. Will the queen’s illness change that?
The queen’s illness spurs an outpouring of support and concern.
The queen remains extremely popular, despite royal family drama.
Queen Elizabeth held an audience at Windsor Castle days before testing positive.
Elizabeth recently marked 70 years on the throne.
.
.
References:
Originally posted at:
https://old.reddit.com/r/ivermectin/comments/sxcl34/queen_elizabeth_tests_positive_for_covid19_what/
Mirrors:
https://saidit.net/s/Ivermectin/comments/8y0f/queen_elizabeth_tests_positive_for_covid19_what/
https://saidit.net/s/Ivermectin2/comments/8y0g/queen_elizabeth_tests_positive_for_covid19_what/
Substack:
https://stereomatch.substack.com/p/queen-elizabeth-tests-positive-for
.
The wiki for r/ivermectin sub-reddit is not visible (restrictions due to quarantine). However, a mirror is maintained at:
https://saidit.net/s/Ivermectin2/wiki/index
.
FLCCC I-MASK+ protocol: https://covid19criticalcare.com/covid-19-protocols/i-mask-plus-protocol/
FLCCC MATH+ protocol: https://covid19criticalcare.com/covid-19-protocols/math-plus-protocol/
FLCCC MATH+ extended PDF: https://covid19criticalcare.com/wp-content/uploads/2020/12/FLCCC-Protocols-%E2%80%93-A-Guide-to-the-Management-of-COVID-19.pdf
FLCCC I-RECOVER protocol for long haulers (and post-vaccine issues): https://covid19criticalcare.com/covid-19-protocols/i-recover-protocol/
.
.
Acknowledgements
Thanks to feedback from friends on Twitter - some clarification sections were added to above text:
Amaresh Kumar: https://twitter.com/amareshskumar
Vijay Gupta: https://twitter.com/OutOfTheDarkAge
Dr Gustavo Aguirre Chang: https://twitter.com/Aguirre1Gustavo
Ketan Shah: https://twitter.com/Thinkerks
Dr A K Chaurasia: https://twitter.com/drakchaurasia
Dr Darrell DeMello: https://twitter.com/DarrellMello
.
Twitter thread: https://twitter.com/stereomatch2/status/1495518722831888387